A domestic animal may be exposed to rabies if it has:
- come into contact with a bat
- been bitten by a wild animal
- been bitten by a domestic animal displaying abnormal behaviour
If a domestic animal is presented to a veterinary practice after a potential rabies exposure, follow the steps below:
- Perform wound decontamination and other patient care if indicated.
- Gather information on the exposure event:
- document event details such as offending species and any observations of their health and behaviour, location, time of day, circumstances, other animals involved, and outcome for the offending animal
- determine the category of rabies risk posed by the offending animal (see below)
- Determine the rabies vaccination status of the exposed animal(s).
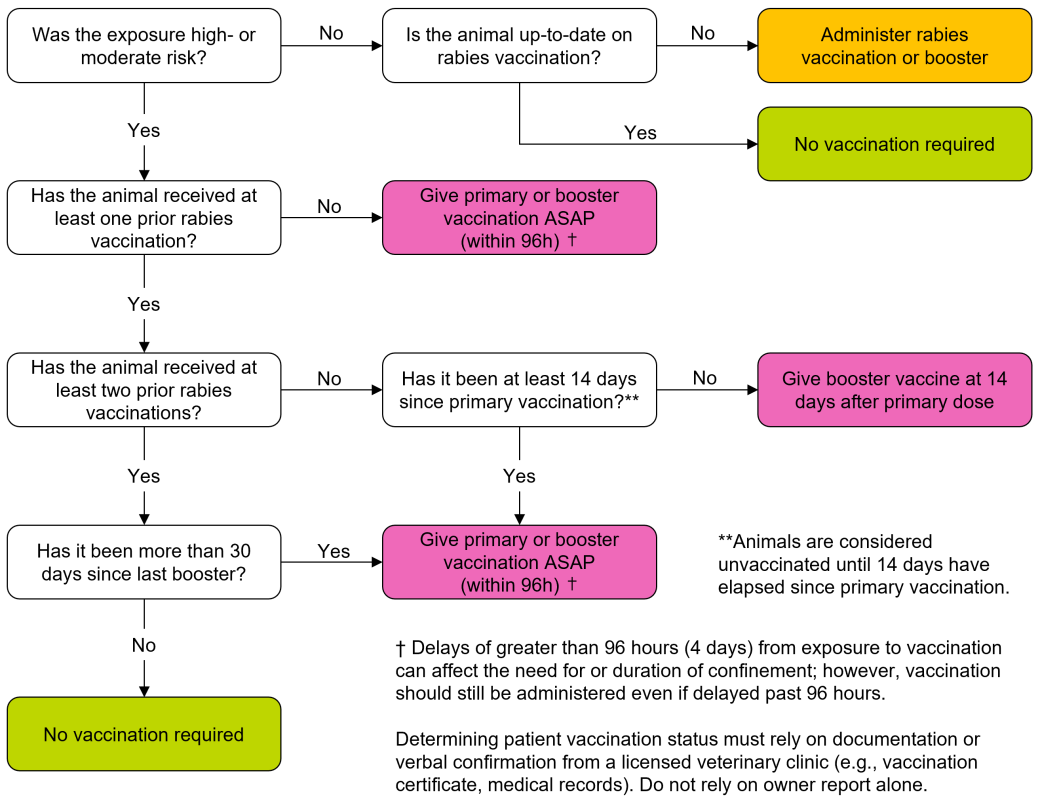
- Administer post-exposure rabies vaccination (see Figure 1 below).
- After a high- or moderate-risk exposure:
- Post-exposure vaccination must occur promptly. Delays of greater than 96 hours (4 days) from the time of exposure may affect the need for or duration of quarantine; however, vaccination should still be administered even if delayed past 96 hours.
- Administer rabies vaccination, even if the exposed animal is fully/currently vaccinated against rabies. If the animal has had at least 2 prior rabies vaccinations administered according to the manufacturer’s directions and the most recent vaccination was within 30 days of the exposure event, a booster vaccination is not required.
- Vaccinate against rabies even if the exposed animal is less than 12 weeks of age. An additional vaccination will be required after 12 weeks of age in accordance with the manufacturer’s directions.
- After a low-risk exposure:
- Vaccinate if the animal is out-of-date or unvaccinated, ideally within 96 hours.
- If a domestic animal may have been exposed to rabies and has bitten a human (for example, Good Samaritan assisting injured domestic animal), provide post-exposure vaccination to the animal and follow the guidance in the section above: Potential exposure of a human. Do not delay vaccination of an exposed animal due to concurrent human exposure.
- Preserve the offending animal carcass (if applicable) in case testing is required
- Rabies Program staff will typically arrange testing of available carcasses for high- and moderate-risk exposures if the exposed animal is unvaccinated or out-of-date (depending on the number of prior rabies vaccinations and when they were last vaccinated).
- Inform and advise the owner about rabies
- Discuss risks, routes of exposures, vaccination, clinical signs and incubation period.
- Request that the owner contact a veterinary clinic or the Alberta Rabies Program if they observe signs of disease in their animal.
- Rabies prevention and control is available as a resource.
- Report all high- and moderate-risk exposures to domestic animals to the Alberta Rabies Program:
Risk of rabies exposure in Alberta based on species and behaviour of the offending animal
High-risk
- bat
- any mammal exhibiting abnormal behaviour or disease (regardless of species)
Moderate-risk
- carnivore, raccoon or skunk with no indications of abnormal behaviour or disease
Low-risk
- non-carnivorous mammal except raccoon or skunk (for example, muskrat, beaver) with no indications of abnormal behaviour or disease
- domestic animal with no indications of abnormal behaviour or disease; risk can be further assessed in these situations by determining the vaccination status of the offending animal and requesting the owner to report any signs of disease in the offending animal that occur within 10 days of the incident
Rabies program staff use these categories of risk for the management of domestic animals potentially exposed to rabies in Alberta. Human exposure assessment is managed by public health under the guidance of a Medical Officer of Health. Potential human exposures are to be reported as indicated in the section above: Potential exposure of a human.
These categories reflect the risk of rabies virus transmission from offending species to domestic animals in Alberta only; they do not apply to other jurisdictions. Bats are currently the only rabies reservoir in Alberta. Spillover of rabies virus from bats to other species does occur, but it is much less common than in jurisdictions where the virus is maintained in foxes, skunks or raccoons. For more information, see Rabies in animals.
Abnormal behaviour or signs of disease
Consider the following when evaluating the behaviour of a wild animal that has bitten a domestic animal:
- whether the time of day or location of the encounter were unusual for the species involved
- the animal’s mentation, movement and general appearance
- whether the encounter was provoked (for example, did the offending animal attack or was it defending itself)
- the duration of the encounter and whether the offending animal attempted to escape
If the offending animal has died, the condition of the carcass (for example, body condition, hair coat, presence of wounds) may provide indications of its health prior to death. If the interaction was not observed, it may also provide indication of the time since death, which is particularly relevant when a pet finds a dead bat. Maintain the carcass in case testing is required. Appropriate protective equipment, including gloves, should be worn if the carcass must be handled.
Figure 1. Rabies vaccination after exposure decision tree
After reporting a domestic animal exposure
The following pertain to high- and moderate-risk exposures of domestic animals.
- Fully vaccinated cats, dogs and ferrets that receive a booster vaccine within 96 hours after exposure will not require quarantine.
- Cats, dogs and ferrets that are unvaccinated or do not receive a booster vaccination promptly after exposure may require a 3- to 6-month quarantine as determined by Alberta’s Public Health Veterinarian:
- if the offending animal is available, the test result will direct case management
- if the offending animal is not available or the sample is determined to be unfit for testing, the need for and duration of quarantine will be determined based on a risk assessment conducted by the Public Health Veterinarian
- Animals that are overdue for rabies booster vaccination will be evaluated on a case-by-case basis. In a majority of cases, a quarantine will not be required in previously vaccinated but out-of-date animals provided they receive a booster vaccination promptly after exposure.
- Management and quarantine following exposure of other domestic animals will depend on the species involved and their intended use.